What is a cardiac MRI?
Magnetic resonance imaging (MRI) is a diagnostic test that uses a powerful magnet and radio wave pulses to create detailed images of body tissue. The test does not require entering the body (it is noninvasive). Cardiac MRI produces images of the heart as it is beating, allowing doctors to clearly see the size and shape of the chambers, the movement of the muscle wall, and the flow of blood.1 It may also be used to assess the ejection fraction, a measure of the heart’s ability to pump blood.2 Cardiac MRI may done with or without contrast dye (used to provide images that are more detailed).
A special MRI technique using contrast dye detects damaged or scarred areas of the heart muscle that can impair the heart’s ability to pump and lead to heart failure. Called delayed-enhancement cardiac MRI, this technique uses a dye that cannot enter healthy heart muscle cells but is absorbed by damaged cells, which show up as bright, motionless areas on the MR image. This technique is used to evaluate heart damage that may have been caused by heart attack, coronary artery disease, or disease of the heart muscle itself.
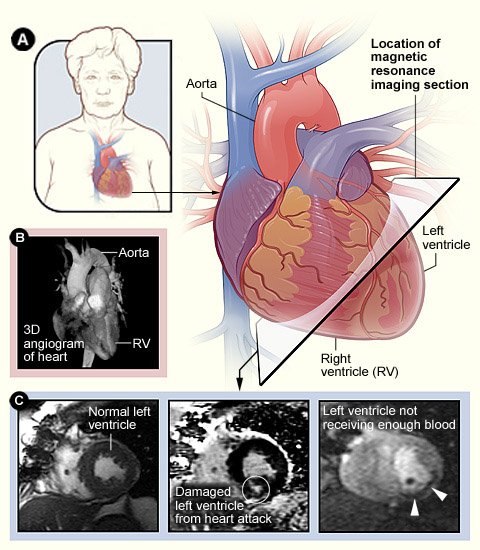
Figure A: Illustration of the heart’s position in the body (top left) and illustration of the heart section (right) shown in the MRI images in Figure C (right).
Figure B: an MR angiogram.
Figure C: MRI images of a normal left ventricle (left), a left ventricle damaged from heart attack (center), and a left ventricle that isn’t getting enough blood from the coronary arteries (right).
Source: NHLBI
Who might have a cardiac MRI?
Although cardiac MRI is more accurate than echocardiography, echo is the standard initial test to measure ejection fraction, mainly because it is fast, widely available, and can be performed if you have an implanted metal device such as a pacemaker or defibrillator. When the echocardiogram is inadequate or inconclusive, cardiac MRI may be used to evaluate ejection fraction (as long as you do not have an implanted metal device).3,4
In hospitals where it is available, cardiac MRI is an effective test for diagnosing heart failure. It can show whether the walls of the heart are enlarged or thickened and if they are contracting and relaxing normally. The test can also provide clues as to what caused the heart failure, such as heart muscle damaged by lack of oxygen resulting from coronary artery disease or heart attack. Knowing the cause of your heart failure helps your doctor determine the best treatment for you. In people with heart failure caused by a heart attack, cardiac MRI can show how much heart tissue has been damaged permanently and how much can still be saved.5
How do I prepare for a cardiac MRI?
You may be required to wear a special gown during the test. Metallic objects can interfere with the magnetic field of the MRI scanner, so before you enter the scanner room you should have all metal removed from your clothing and body. You will need to remove:
- Jewelry, watches, pins, hairpins, metal zippers
- ATM and credit cards
- Hearing aids, dentures, eyeglasses
- Pens, pocket knives
If you have an implanted defibrillator, cochlear (inner ear) implant, or have had a metal clip implanted in your brain to treat an aneurysm, you should not be scanned and should not enter an MRI exam room.
You should inform the technician if you have any of the following in or on your body because they may interfere with the scan or pose a risk:
- Stent implanted in the arteries of your brain or neck
- Intrauterine device (IUD)
- Artificial heart valves
- Implanted electronic device, including a heart pacemaker
- Artificial limb or metallic joint prosthesis
- Implanted nerve stimulators or drug infusion ports
- Tooth fillings, braces, metal pins, screws, plates, or surgical staples
- Metallic-based tattoos
You will usually be provided with a questionnaire that lists all potentially dangerous objects.
Tell your doctor if you are or may become pregnant, because the effects of an MRI on the fetus are not clear. If you are having a test that uses a contrast dye, be sure to tell your doctor if you have kidney problems or have ever had an allergic reaction to shellfish or to the contrast dye or iodine.
What happens during a cardiac MRI?
Photograph of a patient on the sliding table outside of the MRI machine. The table slides inside the tunnel for the scan.
You will lie on your back on a narrow, sliding table. The technician will slide the table into the large tunnel of the MRI scanner using an automatic control. You will be alone in the exam room during the scan; however, the technician will be able to see you through a window from an adjacent room and hear and speak with you through a two-way intercom. Inside the scanner, you will hear loud humming or thumping noises as the machine takes each picture. Earplugs or headphones are usually provided. You may also experience a slightly warm feeling in the area of your body that is being scanned. This is normal, but if it feels uncomfortable, tell the technician.
It is very important that you lie completely still and hold your breath while each scan is being done because movement can blur the image. You can relax between each set of images, but try not to move too much. If you have a serious problem with being in narrow or closed spaces and cannot hold still, you may be given a sedative to help you relax.
If you are having a scan that requires contrast dye, the dye will be injected through an IV in your hand or arm, usually after taking an initial set of images. You may experience coolness and a flushed sensation for a minute. After the dye injection, more images are taken.
The test usually takes about 45 minutes to an hour.
What happens after a cardiac MRI?
After the scan is completed you may be asked to wait while the technician reviews the images and makes sure no more scans are needed. If you have received a medication to help you relax, you will need to rest until the effect wears off and should avoid driving. Nursing mothers who have MRI with contrast dye should wait 36 to 48 hours before breastfeeding because the dye can pass into breastmilk and may be harmful to the baby; milk produced during this period should be discarded.
The images will be reviewed by a radiologist, who will send the results to your doctor. Your doctor will discuss the results with you.
What do the results of a cardiac MRI mean?
An MRI test shows how well your heart is working. Your doctor will check your heart’s pumping ability by measuring the ejection fraction and looking for any irregularities in the movement and size of the heart muscle wall. An MRI can also show the difference between muscle tissue that has been damaged by coronary artery disease or a heart attack and muscle tissue damage caused by other conditions. If you have had a heart attack, an MRI can show which of the affected heart muscle areas may be saved by restoring blood flow to that area.
What are the risks of a cardiac MRI?
MRI is safe and usually painless. There have been no reports of harmful effects from the magnetic field or radio waves. Unlike regular x-rays, MRI tests do not use ionizing radiation.
The dye used in some MRI tests is relatively safe compared with the iodine-based dye usually used for angiograms, and allergic reactions are rare. If you are given medication to help you relax, there is a slight risk of excessive sedation, but your heart rate and breathing will be carefully monitored.
References
- Hunt SA. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol. September 20, 2005 2005;46(6):e1-82.
- Lima JA, Desai MY. Cardiovascular magnetic resonance imaging: current and emerging applications. J Am Coll Cardiol. Sep 15 2004;44(6):1164-1171.
- Kuhl HP, Spuentrup E, Wall A, et al. Assessment of myocardial function with interactive non-breath-hold real-time MR imaging: comparison with echocardiography and breath-hold Cine MR imaging. Radiology. Apr 2004;231(1):198-207.
- White JA, Patel MR. The role of cardiovascular MRI in heart failure and the cardiomyopathies. Cardiol Clin. Feb 2007;25(1):71-95, vi.
- Prasad SK, Kotwinski P, Assomul R. The role of cardiovascular magnetic resonance in the evaluation of patients with heart failure. Expert Rev Cardiovasc Ther. Jan 2004;2(1):53-59.





