What is aortic disease?
Aortic disease is a form of peripheral artery disease that affects the aorta, the largest artery in the body. The aorta is about the thickness of a garden hose and runs from your heart through your chest and abdomen, carrying oxygen-rich blood from the heart’s main pumping chamber (the left ventricle) and distributing it to the smaller arteries that carry blood to the rest of the body.
The most common problem in the aorta is called an aortic aneurysm. An aneurysm is a bulging out of the artery wall, caused by a weakened or diseased artery that stretches like a balloon under the pressure of blood pumped from the heart. These bulges grow in size over time, and without treatment they may eventually rupture, causing massive internal bleeding that usually results in death. In addition to the risk of rupture, aneurysms are also dangerous because they can cause blood clots to form, which may break off and block a blood vessel in another part of the body.
There are two main types of aortic aneurysms, based on where they occur:
- Thoracic Aortic Aneurysms (TAA) – occur in the upper part of the aorta that runs through the chest (behind the heart). TAAs account for 1 in 4 aortic aneurysms.
- Abdominal Aortic Aneurysms (AAA) – occur in the lower part of the aorta that runs through the abdomen, just below where the kidney (renal) arteries branch off. AAAs account for 3 in 4 aortic aneurysms.
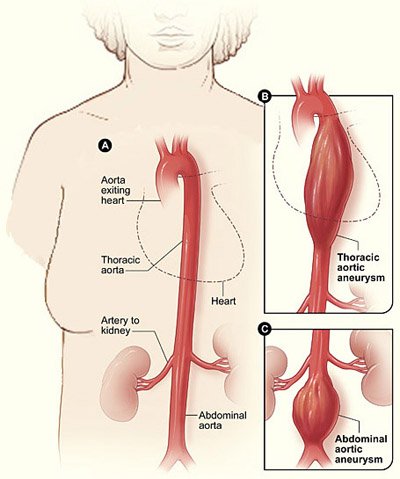
A: A normal aorta. B:Thoracic aortic aneurysm (TAA), located behind the heart. C:Abdominal aortic aneurysm (AAA) located below the arteries that supply blood to the kidneys.
When aortic aneurysms rupture, they are fatal as much as 90% of the time.1 Each year nearly 14,000 Americans die of aortic aneurysms, including more than 5000 women.2,3 Fortunately, rupture can usually be prevented if the aneurysm is detected early. Lifestyle changes and medications can slow the growth of smaller aneurysms, and repair procedures can reinforce or replace the artery wall and prevent a larger aneurysm from bursting.
What causes aortic disease?
The most common cause of aortic aneurysms is damage to the aorta walls caused by atherosclerosis, the gradual buildup of fatty deposits called plaque. This same process causes a heart attack or chest pain when it narrows or blocks blood vessels in the heart, and a stroke if it blocks blood vessels in the head or neck. However, doctors don’t know all the reasons that women end up with aortic aneurysms.
The aorta needs to be very elastic to expand when a large volume of blood is pumped into it from the heart, and then relax as the blood flows through. Atherosclerosis makes the walls of the aorta less flexible and causes inflammation, which leads to a weakening of the artery walls. Tobacco smoking and problems with the artery lining can also contribute to a breakdown of the aortic wall. Over time, the force of blood flowing through the aorta causes a weak spot to bulge out like a balloon, forming an aneurysm.
Aortic aneurysms may also be caused by chest injury from a car accident or fall, or genetic disorders that affect the makeup of the blood vessel wall.
What are the symptoms of aortic disease?
Aortic aneurysms usually do not cause symptoms in the early stages. However, as they grow bigger they may cause symptoms when they put pressure on nearby organs.
Symptoms of thoracic (chest) aortic aneurysm:
- Deep, aching or throbbing chest pain
- Back pain
- Cough or shortness of breath
- Hoarseness, difficult or painful swallowing
Symptoms of abdominal (belly) aortic aneurysm:
- Abdominal pain or discomfort; can be constant or come and go
- Pain in the chest, abdomen, lower back, or flank that can spread to the buttocks, groin, or legs; lasts for hours or days
- A pulsating feeling in the abdomen
- Feeling of fullness after minimal food intake
- Fever or weight loss
- Rarely, you may have pain, discoloration, or sores on the toes or feet because of a plaque or a blood clot that has broken off from the aneurysm and become lodged in a blood vessel in your leg
If an aortic aneurysm grows large enough, it may break open (rupture), causing severe internal bleeding that is deadly if not treated immediately. If you have any of these signs of a ruptured aortic aneurysm, call 9-1-1 immediately:
- Sudden severe chest or upper back pain, often described as a tearing or ripping sensation
- Feeling dizzy or lightheaded or passing out
- Weakness or trouble standing up
- Confusion, anxiety, loss of alertness
Who is at risk for aortic disease?
Aortic aneurysms are 5 to 10 times more common in men than in women. They become more common in both sexes as you get older. In women aged 45 to 54, fewer than 1 in 1000 have an AAA, compared with more than 1 in 100 men. At ages 75 to 84, 5% of women have them, compared with 13% of men.1
In addition to older age and male gender, people with high blood pressure, high cholesterol, or who smoke are at higher risk for aortic aneurysms. Smoking is one of the strongest risk factors for aortic aneurysms because it directly damages the arteries and contributes to other conditions like atherosclerosis and high blood pressure. Women and men who smoke are 5 times more likely than nonsmokers to have an aortic aneurysm, and as many as 3 in 4 people with large AAAs are current or former smokers.4 Because atherosclerosis affects all the blood vessels in your body, if you have artery disease elsewhere (such as coronary artery disease, carotid artery disease or stroke, or peripheral artery disease in the legs) you are likely to have atherosclerosis in your aorta as well, and may be at risk for an aortic aneurysm.1
Aortic aneurysms also have a genetic component in some people, and you are at risk if an immediate family member (parent or sibling) has had an aortic aneurysm. One in 4 people with an AAA have an immediate relative with the disease.5



