Diagnosis of Deep Vein Thrombosis
Deep Vein Thrombosis, or DVT, is the formation of one or more blood clots in the body’s large veins (vessels that carry blood back to the heart), usually in the lower leg or calf. These clots can partially or completely block the vein, causing pain, swelling, and tenderness.
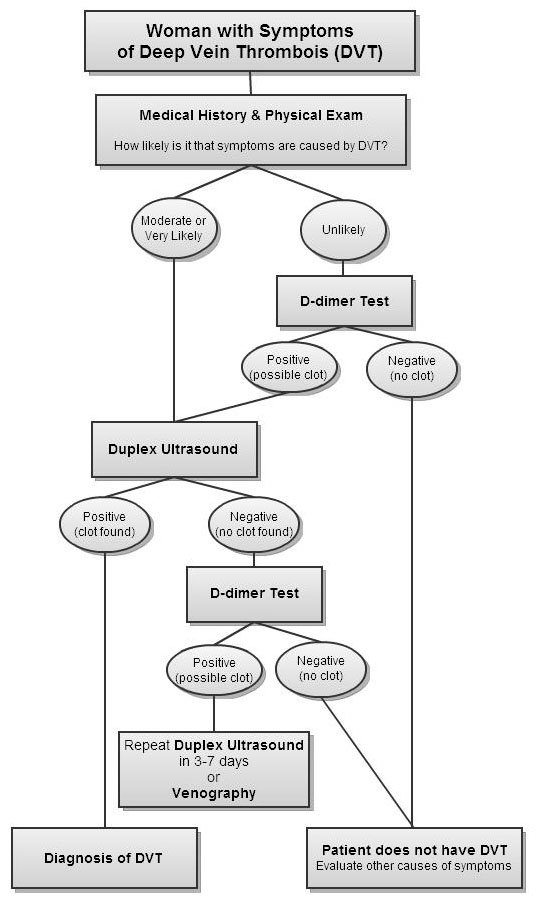
If you have any symptoms of vein disease (such as swelling, pain, tenderness, or warmth in one leg or along a leg vein), contact your doctor immediately so she or he can investigate whether you have blood clots in the veins of the legs. Early diagnosis and treatment of DVT can prevent vein damage and a potentially deadly pulmonary embolism. An evaluation for DVT consists of:
- A medical history and physical examination to check for signs of blood clots and determine your overall blood clot risk
- A blood test called the D-dimer test, which can be used to quickly rule out blood clots
- Imaging tests to look at the structure of the veins in the legs and blood flow through them and identify any clots
Medical History & Physical Examination
If you have the symptoms of DVT, your doctor will ask you about your medical history and perform a physical examination to determine your risk for DVT and look for other causes of your symptoms.
A medical history includes a complete review of any medical conditions you have (especially those that make you more likely to develop blood clots) and any medications you are taking (including prescription drugs, over-the-counter medications, and dietary supplements). Certain medications, such as birth control pills and hormone replacement therapy can make women more likely to develop clots.
Your doctor will also review your medical history for any recent surgeries or hospitalizations. Vein injuries during surgery or long periods of immobility in a hospital or nursing home can trigger blood clots in women who are already at risk. See Am I at Risk for DVT for information on other characteristics and conditions (called risk factors) that make you more likely to develop blood clots in the veins.
During a physical examination for DVT, your doctor will examine your legs for varicose veins and swelling or tenderness in the leg veins, and ask you about any leg pain you have been experiencing. Women with DVT often experience pain or tenderness in one leg that only happens when standing or walking. However, because the symptoms of DVT can be caused by many other conditions, a physical examination is rarely able to diagnose DVT on its own. Instead, your doctor will evaluate your overall risk of blood clots together with any symptoms and decide if further tests are necessary.
D-dimer Test
A blood test called the D-dimer test is often the first test in women with a suspected DVT. The D-dimer test measures the levels of a specific protein in the blood that is produced when blood clots are broken down by the body. If your doctor thinks you are at low risk for DVT and the D-dimer test is negative (there is no evidence of a clot), you are very unlikely to have a DVT.1
If the D-dimer test is positive or you are at high risk for DVT because of other conditions, your doctor will order an imaging test to examine the veins and locate any blood clots.
Imaging Tests
The first imaging test used to diagnose DVT is usually an ultrasound of the leg. This fast, simple, painless test uses sound waves (like those used to view the fetus during pregnancy) to produce images of the veins. Ultrasound is very accurate at diagnosing blood clots in the upper legs, but may miss some clots in the calves and the pelvis.
If an ultrasound is normal or inconclusive but your doctor still suspects a DVT, you may need to have the test repeated in 3 to 7 days. Another option is to have a more detailed test called venography.2
Venography is the gold standard test for the diagnosis of DVT. A dye is injected into a vein in the foot, which highlights the leg veins on an X-ray image as the blood is carried back to the heart. A blood clot will appear as an area inside the leg veins where the dye did not penetrate. In some cases, an alternate version of venography that uses a CT scanner and an injected dye ( CT venography) may be used to diagnose DVT.
The venography test involves X-rays and an injected dye, and sometimes the insertion of a long, thin tube called a catheter (CATH-eh-ter) into the blood vessels. Because of these risks, it is typically only used after other imaging tests have failed to find a clot. Venography may be necessary in very obese women or women with severe swelling because these conditions can block the sound waves used during an ultrasound test.
DVT Diagnosis Overview
Diagnosis of Pulmonary Embolism
One in three women with a blood clot in the veins of the leg (DVT) suffer a serious complication called pulmonary embolism (PE).3 This happens when part of the blood clot breaks off and travels through the bloodstream, eventually blocking an artery that supplies blood to the lungs. PE is extremely serious and often causes sudden death, but if it is diagnosed quickly medication can be used to break up the clot and prevent new clots from forming, restoring blood flow to the lungs. You should learn to recognize the symptoms of pulmonary embolism and call 9-1-1 if you experience any of them:
- Unexplained shortness of breath or difficulty breathing
- Rapid heartbeat, sweating, and/or sharp chest pain, especially during deep breathing
- Coughing up blood
- Dizziness or passing out
An evaluation for pulmonary embolism will include:
- A medical history and physical examination to check for signs of blood clots and determine your overall blood clot risk
- A blood test called the D-dimer test, which can be used to quickly rule out blood clots
- Imaging tests to look at the structure of the arteries in the lungs and blood flow through them and identify any clots. These tests may also be used to look for a blood clot in the leg veins that could have caused the pulmonary embolism.
Medical History & Physical Examination
Women with a pulmonary embolism usually arrive at the emergency room because the symptoms of pulmonary embolism are easily recognizable as a medical emergency:
- Unexplained shortness of breath or difficulty breathing
- Rapid heartbeat, sweating, and/or sharp chest pain, especially during deep breathing
- Coughing up blood
- Dizziness or passing out
A woman with any of these symptoms will be rapidly evaluated for PE so doctors can begin immediate treatment with blood thinning drugs. Doctors will also review your medical history to determine if a blood clot is the likely cause of your symptoms. Some other conditions that make blood clots more likely to form include:
- Recent cancer treatment
- A long period of staying still (such as after surgery or an injury)
- History of DVT or pulmonary embolism
- Inherited blood clotting problems
To decide how to proceed, doctors will take into account your overall blood clot risk and how closely your symptoms match the symptoms of pulmonary embolism. If you have the symptoms of severe PE, you may receive immediate treatment with blood thinning drugs because the risk of delaying treatment for further tests is too great.
D-dimer Test
The first test used to diagnose pulmonary embolism is often a blood test called the D-dimer test. The D-dimer test measures the levels of a specific protein in the blood that is produced when blood clots are broken down by the body. A negative D-dimer test can quickly rule out a blood clot as the cause of symptoms, but a positive D-dimer test is not enough to diagnose PE on its own and further tests will be needed.
If your symptoms match the symptoms of a PE, even if the D-dimer test is negative, your doctor will refer you for imaging tests to attempt to locate the clot.
Imaging Tests
The main imaging test to diagnose a pulmonary embolism is a CT angiogram. This test uses a CT scanner and an injected dye to produce detailed images of the lung arteries and the blood flow through them, and can identify if a clot is blocking blood flow to the pulmonary arteries.
If the CT angiogram does not find a clot, but your doctor still thinks your symptoms are caused by PE, a duplex ultrasound test of the veins in the legs may be performed. This test can diagnose a clot in the veins that could be the source of the pulmonary embolism. In some cases, a CT venogram test to look for a DVT may be performed at the same time as the initial CT angiogram test. If an ultrasound or venography find a DVT, it is likely that part of the clot broke off and caused a PE. Women being evaluated for pulmonary embolism may also have other tests to look at for heart and lung problems that could be causing the symptoms, such as a chest x-ray or ECG.
Pulmonary Embolism Diagnosis Overview
What happens next?
If you are diagnosed with DVT or pulmonary embolism, medication will be used to break up the clot and/or prevent new clots from forming. You may also need additional medications and lifestyle changes to prevent future blood clots. See Treatment for Deep Vein Thrombosis & Pulmonary Embolism (coming soon) for more on how blood clots are treated, and see Living with Vein Disease (coming soon) for tips on preventing future clots.
References
- Wells PS, Anderson DR, Rodger M, et al. Evaluation of D-Dimer in the Diagnosis of Suspected Deep-Vein Thrombosis. N Engl J Med. September 25, 2003 2003;349(13):1227-1235.
- Kearon C, Ginsberg JS, Douketis J, et al. A randomized trial of diagnostic strategies after normal proximal vein ultrasonography for suspected deep venous thrombosis: D-dimer testing compared with repeated ultrasonography. Ann Intern Med. Apr 5 2005;142(7):490-496.
- Kearon C. Natural history of venous thromboembolism. Circulation. Jun 17 2003;107(23 Suppl 1):I22-30.





